Understanding Pain Behind the Knee: Managing & Treatment
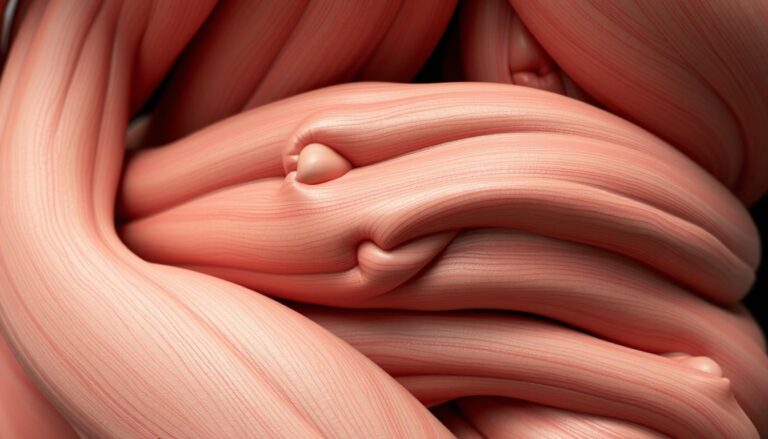
Pain behind the knee often feels like a quiet warning. It can stem from strained muscles around the joint or from issues inside the knee, like meniscal tears, bursitis, tendonitis, or ligament injuries. Activities that involve repetitive motion and overuse are common culprits. Additionally, osteoarthritis and age-related wear contribute to posterior knee pain as people age.
Posterior knee pain affects a broad spectrum of individuals. This includes athletes who engage in high-intensity activities, weekend gardeners, and office workers who spend extended periods sitting. Most cases can be managed with rest and simple treatments. However, if knee pain persists for more than a few days, seeking medical advice is crucial. Early evaluation is key to effective knee pain treatment, addressing both symptoms and underlying causes.
Key Takeaways
- Pain behind the knee can stem from muscles, tendons, bursae, cartilage, or ligaments.
- Posterior knee pain grows more common with age and with repetitive activities.
- Short-term home care often helps, but persistent pain needs medical assessment.
- Effective knee pain treatment balances symptom relief and addressing underlying damage.
- Timely diagnosis improves outcomes and limits long-term joint problems.
Overview Of Posterior Knee Pain And Who It Affects
Posterior knee pain is discomfort at the back of the knee, distinct from issues in the front or general knee areas. Symptoms range from a dull ache to sharp pains, accompanied by stiffness, swelling, and sometimes grinding or popping sounds. The causes include soft-tissue injuries, tendon problems, and joint degeneration. Identifying the source is crucial for effective pain management.
Definition And Scope Of Posterior Knee Pain
This term encompasses pain at the back of the knee, which can occur suddenly after a strain or gradually from overuse. Acute incidents include meniscal tears and ligament sprains. Chronic issues, such as tendinitis, bursitis, and osteoarthritis, lead to persistent pain. Grasping the causes of knee pain helps in pinpointing appropriate treatments and next steps.
Who Is At Risk: Age, Activity Level, And Occupations
Age significantly increases the risk of posterior knee pain due to wear-and-tear and osteoarthritis. Active individuals, especially those who engage in running, jumping, or rapid training increases, face higher risks of overuse and tendinitis.
Jobs requiring prolonged kneeling, repeated squatting, heavy lifting, or long standing periods heighten the risk of bursitis and muscle strain. Sedentary lifestyles can lead to muscle imbalances, altering biomechanics and increasing the risk of discomfort behind the knee.
When To See A Healthcare Provider
Seek medical evaluation if pain persists for more than a few days, intensifies, or hampers walking, stair climbing, or daily activities. Warning signs include severe swelling, instability, fever, inability to bear weight, or sudden sharp pain after trauma. These indicators signal the need to consult a doctor, as ignoring knee pain can have serious consequences.
Early diagnosis, targeted examination, and imaging when necessary guide treatment. Patients who seek medical attention for posterior knee pain often experience shorter recovery times and clearer paths for managing their pain.
Common Knee Pain Causes Behind The Knee
Pain behind the knee can stem from various sources. Some issues flare up after a run, while others develop gradually with age. Below, we outline common causes and their typical sensations.
Muscle Strains And Overuse Injuries
Repetitive stress from activities like running, jumping, or prolonged kneeling often leads to overuse injuries knee. Tight hamstrings or calf muscles can tear near the knee, causing muscle strains behind knee. These feel like a dull ache or tightness.
Increased training or poor flexibility can heighten the risk. Rest, gradual stretching, and a cautious return to activity usually help alleviate symptoms.
Tendonitis And Bursitis Affecting The Back Of The Knee
Tendon inflammation from repeated motion manifests as tendinitis knee, with localized pain and morning stiffness. The hamstring and popliteal tendons are frequently affected.
Bursitis behind knee causes swelling and point tenderness due to friction or pressure. Many cases improve with activity modification, cryotherapy, and targeted rehab.
Meniscal Tears And Ligament Injuries Presenting With Posterior Pain
Meniscus tear pain often refers to the back of the joint, especially when the posterior horn is involved. Patients may report popping, catching, or a catching sensation with limited motion.
A ligament injury back of knee, such as a posterior cruciate sprain, often follows a forceful impact or twist. It may cause sharp pain behind the knee plus instability. These injuries sometimes require imaging or specialist care when mechanical symptoms persist.
Osteoarthritis And Degenerative Joint Changes That Cause Pain Behind The Knee
Osteoarthritis knee brings cartilage loss and joint inflammation, presenting as aching in the posterior compartment. Degenerative knee pain grows over months to years and often coexists with muscle imbalance and altered gait.
Long-term wear can feed chronic posterior knee pain, increasing stress on nearby tendons and bursae. This makes simple tasks like climbing stairs uncomfortable.
Recognizing Symptoms Of Discomfort Behind Knee
Pain behind the knee manifests in various ways. Some feel a persistent ache after a long day. Others experience tightness or stiffness after sitting for a while. These symptoms help identify the cause and guide the next steps.
Typical Symptoms: Aching, Stiffness, Swelling, Grinding Or Popping
Many report a deep ache behind the knee that disrupts sleep. Stiffness often occurs after rest, making the first steps painful. Visible swelling back of knee may appear as a soft bulge or firmness behind the joint.
Some feel sensations of grinding or popping during movement. These noises can be accompanied by discomfort when straightening or bending. Tracking these signs is crucial for describing them clearly at a clinic visit.
Activity-Related Patterns: Worse With Bending, Squatting, Stair Climbing
Activity-related knee pain tends to worsen when the joint is loaded. Many patients experience knee pain worsening with bending or deep squats. Pain also rises while rising from a chair or when kneeling.
Stair climbing knee pain is a common indicator of strained posterior structures. Symptoms may build throughout the day and peak after exercise or long walks. Noting which actions trigger pain helps clinicians pinpoint causes.
Red Flags: Severe Swelling, Instability, Fever, Or Inability To Bear Weight
Watch for red flags knee pain that require urgent attention. Sudden, severe swelling back of knee, a knee that gives way, or an inability to put weight down are warning signs. Fever paired with joint pain raises concern for infection.
Emergency knee pain signs include intense instability or a knee that cannot be straightened. When to seek care knee becomes critical if symptoms are sudden or severe. Prompt evaluation prevents complications.
| Symptom | How It Feels | When It Matters |
|---|---|---|
| Deep aching | Persistent, dull pain behind knee | Worse after activity or at night; suggests overuse or degeneration |
| Stiffness | Difficulty bending or straightening | Notable after rest; may limit daily tasks |
| Swelling back of knee | Visible bulge or tightness | Acute or progressive swelling needs assessment |
| Grinding/popping | Clicking sensations with motion | May indicate cartilage or meniscal involvement |
| Knee pain worse with bending | Pain spikes during squats, kneeling, or sitting-to-standing | Activity-related knee pain pattern guides treatment choice |
| Stair climbing knee pain | Pain increases when ascending or descending stairs | Common in posterior or patellofemoral issues |
| Red flags knee pain / emergency knee pain signs | Severe swelling, fever, instability, inability to bear weight | Seek immediate care; possible infection, fracture, or major tear |
How Clinicians Diagnose Pain Behind The Knee
Diagnosing knee pain starts with a detailed conversation and a hands-on examination. Clinicians delve into the onset of symptoms, the activity at the time of injury, and how pain changes with movement. They also explore any previous knee issues. This initial discussion sets the stage for further investigation and narrows down potential causes.
Medical History And Physical Exam Focus For Posterior Knee Pain
During the physical exam, providers look for signs of swelling, bruising, and deformity. They assess range of motion, strength, and tenderness in specific areas. Special tests are used to check for injuries to the meniscus or ligaments. Simple tasks help reveal functional limitations.
Combining the medical history with physical findings helps distinguish between soft-tissue and intra-articular problems. This distinction guides the choice of imaging tests.
Imaging Tests: X-Ray, MRI, And When Each Is Indicated
An X-ray is useful for examining bone alignment, osteoarthritis, or fractures. Its availability and speed make it a common first choice for knee pain imaging.
An MRI is preferred for detailed views of menisci, ligaments, tendons, and soft-tissue injuries. It’s crucial for confirming tears and determining their extent, especially when considering surgery or targeted nonoperative treatments.
Ultrasound is useful for evaluating bursae and some tendon issues in real-time. The choice of imaging depends on the clinical suspicion and findings from the physical exam.
When Referral To Orthopedics Or Physical Therapy Is Recommended
Early referral to physical therapy is common for strains, tendinitis, and postoperative rehabilitation. Structured physical therapy can speed up recovery and reduce the risk of future problems.
An orthopedic referral is appropriate for suspected meniscal or ligament tears, persistent pain after conservative treatments, or when surgery might be necessary. Collaboration between primary care, physical therapy, and orthopedics ensures appropriate treatment based on the diagnosis.
| Step | Purpose | Typical Outcome |
|---|---|---|
| Medical history knee pain | Identify onset, activity at injury, symptom pattern | Targets exam and imaging choices |
| Physical exam posterior knee | Assess swelling, ROM, strength, localized tenderness | Suggests soft-tissue vs intra-articular source |
| Knee X-ray | Evaluate bone alignment, arthritis, fractures | Confirms degenerative change or bony injury |
| Knee MRI posterior pain | Visualize menisci, ligaments, tendons | Detects tears and complex soft-tissue injuries |
| Ultrasound | Real-time assessment of bursae and tendons | Useful for guiding injections and dynamic problems |
| Refer to physical therapy knee pain | Rehabilitation, load management, return-to-activity | Improves function and reduces recurrence |
| Orthopedic referral posterior knee | Evaluate for surgery or advanced interventions | Surgical planning or specialist nonoperative care |
Conservative Knee Pain Treatment Options
For many, the initial approach involves simple, effective steps to reduce pain and swelling. These steps also ensure the knee remains mobile to prevent stiffness. A personalized strategy combines home remedies with short-term medical interventions and wise adjustments in activity.
Rest, Ice, Compression, And Elevation Tailored For Posterior Knee Discomfort
Begin with RICE knee pain methods to control swelling in the first 48 to 72 hours. Ice therapy for 15–20 minutes several times a day is beneficial. Additionally, use a compression wrap or sleeve and elevate the leg when sitting or sleeping.
It’s crucial to avoid complete immobilization. Gentle exercises to maintain range of motion after initial pain subsides are recommended. Healthcare professionals often suggest short walks and controlled bending over prolonged bed rest.
Medications For Pain Relief And Inflammation Management
Over-the-counter medications can alleviate symptoms during the healing process. NSAIDs like ibuprofen or naproxen are effective in reducing inflammation and pain for many individuals.
Acetaminophen is an alternative when NSAIDs are not suitable. Topical NSAID gels offer targeted relief behind the knee with fewer systemic side effects. Decisions on long-term use should be made with a healthcare provider, considering individual medical histories.
Activity Modification And Temporary Use Of Assistive Devices
Modifying activities to reduce stress on the knee is essential until pain subsides. Switch high-impact exercises for low-impact alternatives like swimming or cycling to maintain fitness without exacerbating posterior knee pain.
Supportive tools aid in returning to normal activities. A knee brace or sleeve can offer stability during short walks. For severe limping, crutches can help distribute weight while the knee heals.
| Measure | How It Helps | When To Use | Notes |
|---|---|---|---|
| RICE knee pain (rest ice compression elevation knee) | Reduces swelling and acute pain | First 48–72 hours after injury or flare | Combine with gentle motion after initial phase |
| Oral knee pain medications | Controls pain and inflammation systemically | Short-term for flare-ups or acute injuries | Consider contraindications; consult a clinician |
| Topical NSAIDs for knee pain | Local pain relief with fewer systemic effects | Localized posterior knee soreness | Useful for people with GI or cardiac risks |
| Activity modification knee pain | Prevents further irritation and promotes healing | Whenever activities reproduce pain | Plan gradual return-to-activity |
| Knee brace for posterior pain | Provides stability and reduces strain | During walking or rehab exercises | Short-term use advised while strengthening |
| Crutches knee pain | Offloads weight from the injured limb | Marked limp or inability to bear weight | Use temporarily until pain and function improve |
Rehabilitation And Managing Knee Pain With Exercises
Targeted movement helps people overcome pain behind the knee and return to daily activities. A simple plan combines flexibility exercises, gentle joint drills, and strength training. Progress is steady, guided by pain levels and real-world goals like climbing stairs or returning to sports.
Stretching And Mobility For Posterior Knee Comfort
Start with controlled stretches for the hamstrings and calf muscles to ease tension where the knee connects to soft tissue. Light hamstring stretches knee pain survivors use, performed daily, reduce pull on the back of the knee and help normalize gait.
Include short mobility exercises posterior knee—calf pumps, heel slides, and gentle knee bends—to keep range without aggravating symptoms. Work within pain limits and avoid forcing a deep stretch.
Strengthening Routines To Balance Support
Begin with low-load knee strengthening exercises such as quad sets, straight-leg raises, and glute bridges to strengthen knee muscles without heavy joint stress. Add resistance bands and closed-chain moves when pain allows.
A focused plan will correct muscle imbalances knee by targeting the quads, glutes, and hamstrings. Balanced strength reduces posterior loading and lowers the risk of repeat flare-ups.
Physical Therapy And A Gradual Return-To-Activity Plan
Physical therapists design individualized programs that blend manual therapy, progressive exercise, and movement retraining for managing knee pain PT. They check gait, squat form, and sport patterns to prevent relapse.
Return-to-activity knee rehab follows stages: protect and restore motion, build controlled strength, then add sport- or job-specific drills. Clear benchmarks for flexibility, strength, and pain guide each step.
- Examples of safe early work: isometrics, heel raises, and short stationary cycling.
- Mid-stage: single-leg balance, step-ups, and resisted band work.
- Late-stage: plyometrics, agility drills, and simulated sport moves.
Consistent practice of stretches for back of knee and knee strengthening exercises, paired with ongoing mobility exercises posterior knee, offers long-term gains. Regular check-ins with a clinician support recovery and help the body adapt safely.
Advanced And Procedural Knee Pain Treatment Options
When basic care fails to alleviate persistent discomfort behind the knee, more targeted procedures and technologies become available. Healthcare professionals evaluate symptom patterns, imaging results, and patient goals to recommend the best course of action. They aim to enhance function and reduce pain with the least invasive methods.
When Injections Are Considered
Injections are considered when rest, therapy, and medications no longer provide relief. Corticosteroid injections can quickly reduce swelling and inflammation. Hyaluronic acid injections help by restoring joint lubrication and improving movement for those with osteoarthritis.
Doctors discuss the expected duration of relief, potential side effects, and how injections fit into a comprehensive treatment plan. Some patients opt for repeated injections, while others use them as a temporary solution before more invasive treatments.
Minimally Invasive Procedures And Indications For Surgery
For persistent mechanical symptoms, minimally invasive procedures can diagnose and treat issues with minimal trauma. Arthroscopy allows surgeons to trim torn meniscus, remove loose fragments, or smooth out rough cartilage through small incisions.
More complex surgeries, such as meniscal repair, ligament reconstruction, or joint replacement, are considered for severe structural damage or advanced osteoarthritis. Decisions about knee surgery are based on function, imaging, and how symptoms impact daily life.
Non-Surgical Technology And Alternative Therapies For Managing Knee Pain
Non-surgical treatments for knee pain include a variety of options. Regenerative approaches like platelet-rich plasma and biologics are available in specialized clinics. FDA-approved gel injections target osteoarthritis specifically.
Supportive care includes bracing, shoe inserts, ultrasound, and electrical stimulation. Lifestyle changes like weight loss and low-impact cardio are also effective. Patients often combine these with targeted activity modification programs.
Early consultation with an orthopedist or sports medicine specialist is crucial. They help tailor the right combination of knee pain technology and alternative therapies to individual needs. This conversation focuses on evidence, expected outcomes, and practical steps towards recovery.
Preventing Future Episodes Of Knee Pain
Small changes can significantly improve knee health. Maintaining a healthy weight, choosing low-impact cardio, and adopting good movement habits are key. These actions help prevent knee pain and keep mobility high for years.
Weight Management And Low-Impact Cardio To Reduce Joint Stress
Reducing body weight can greatly reduce joint stress. Each pound lost can decrease the force on the knee by several pounds. This makes weight management a crucial step for many.
Opt for low-impact cardio like cycling, swimming, or using an elliptical. These activities are gentle on cartilage, improve endurance, and help maintain a healthy weight.
Proper Biomechanics, Footwear, And Training Modifications
Good movement is more important than brute force. Proper biomechanics include correct squat depth, hip control, and a well-tuned gait. These habits reduce abnormal loading and tendon stress behind the knee.
Choose footwear that offers support and shock absorption. Brands like Brooks or HOKA are often recommended for supportive running shoes.
Adopt training modifications such as gradual mileage increases, cross-training, and regular rest days. These measures prevent overuse injuries and lower the risk of tendonitis or recurrent posterior pain.
Long-Term Strategies For People With Osteoarthritis Or Chronic Posterior Knee Pain
Managing long-term knee pain involves a mix of exercise, pacing, and regular reviews. A chronic care plan combines strength training with joint protection and symptom tracking. This approach helps maintain mobility.
Strategies for osteoarthritis may include physical therapy, weight control, and targeted interventions to delay surgery. Early adjustments can limit symptom progression and preserve daily function.
Managing chronic posterior knee pain requires routine checks, modest assistive devices, and non-surgical options like guided injections or supervised rehab. These steps support ongoing activity and quality of life.
Conclusion
Pain behind the knee can stem from overuse or more serious issues like meniscal tears and osteoarthritis. Symptoms include aching, stiffness, swelling, and pain that gets worse with bending or climbing. Early detection and a precise diagnostic approach—history, physical exam, and imaging when necessary—are key to effective treatment.
The most effective strategy involves staged care. Begin with rest, ice, and adjusting activities. Then, move to rehabilitation to regain strength and mobility. Many find relief through physical therapy, exercise, and managing weight before resorting to injections or surgery.
Prevention is crucial. Paying attention to biomechanics, wearing proper footwear, and engaging in low-impact cardio can reduce joint stress and lower the risk of recurrence. If symptoms persist, working with a physical therapist or orthopedic specialist is the best way to manage knee pain and maintain joint health.
FAQ
What Causes Pain Behind The Knee?
Posterior knee pain can stem from various sources. Soft-tissue injuries, such as hamstring or calf strains, are common culprits. Overuse, like tendonitis, also plays a significant role. Additionally, inflamed bursae, meniscal tears, ligament sprains, and degenerative conditions like osteoarthritis contribute to the pain. These issues can arise from acute trauma, repetitive stress, or wear-and-tear over time.
Who Is Most Likely To Get Posterior Knee Pain?
Individuals who engage in activities that involve running, jumping, or squatting are at higher risk. This includes athletes and those who suddenly increase their training intensity. Jobs that require frequent kneeling, heavy lifting, or prolonged standing also increase the risk of bursitis and chronic stress. Furthermore, age-related wear-and-tear, such as osteoarthritis, raises the risk as well.
What Symptoms Suggest A Serious Problem?
Severe swelling, sudden instability, fever with knee pain, inability to bear weight, or sharp pain after trauma are red flags. These symptoms may indicate serious issues like infection, major ligament or meniscal tears, or fractures. Immediate medical evaluation is crucial.
How Do Clinicians Diagnose Posterior Knee Pain?
Diagnosis involves a detailed history and physical examination. Clinicians assess range of motion, tenderness, swelling, and perform specific tests for meniscus or ligament injuries. X-rays are used to evaluate bone alignment and osteoarthritis. MRI is preferred for soft-tissue issues, while ultrasound can assess bursae and tendons in real-time.
What Are First-Line Treatments For Back-Of-Knee Pain?
Initial treatment includes modified RICE (rest, ice, compression, elevation) to avoid prolonged immobilization. Short-term use of NSAIDs or acetaminophen for pain management is recommended. Activity modification and assistive supports like knee sleeves are also advised. Early gentle movement and avoiding aggravating activities help prevent stiffness.
When Are Physical Therapy And Exercises Recommended?
Physical therapy is often recommended early for strains, tendinitis, postoperative recovery, and chronic issues. PT focuses on gentle mobility, stretching, and strengthening exercises. It aims to correct biomechanics and reduce recurrence risk through a staged return-to-activity plan.
Are Injections Or Surgery Ever Needed?
Injections, such as corticosteroids for inflammation or hyaluronic acid for osteoarthritis, may be considered when conservative treatments fail. Arthroscopic procedures can address certain meniscal tears or loose bodies. More extensive surgery, like meniscal repair or ligament reconstruction, is reserved for severe structural damage or advanced osteoarthritis after nonoperative measures are exhausted.
How Can I Prevent Recurrence Of Posterior Knee Pain?
Prevention involves maintaining a healthy weight, engaging in low-impact cardio, and correcting biomechanics and footwear. Gradual training progressions and targeted strength and flexibility exercises are key. Regular monitoring and early intervention for flare-ups help preserve function and delay degenerative progression.
How Long Should I Wait Before Seeing A Healthcare Provider?
If pain persists beyond a few days, worsens, limits walking or stair climbing, or is accompanied by swelling or mechanical symptoms, seek medical attention. Early evaluation with history, exam, and imaging when indicated helps identify the cause and guide appropriate treatment to prevent further damage.
What Lifestyle Changes Support Long-Term Knee Health?
Maintaining a healthy weight reduces joint load. Choose low-impact cardio activities and strengthen core and lower-limb muscles. Prioritize flexibility of hamstrings and calves, and adopt proper lifting and squat techniques. These measures lower the risk of osteoarthritis progression and recurrent posterior knee discomfort.